
伤口世界
- 星期四, 05 9月 2024
Biological mechanisms of aging predict age-related disease co-occurrence in patients
Helen C. Fraser1 | Valerie Kuan2,3,4 | Ronja Johnen5 | Magdalena Zwierzyna6 | Aroon D. Hingorani3,4,6 | Andreas Beyer5,7 | Linda Partridge1,8
1 Department of Genetics, Evolution and Environment, Institute of Healthy Ageing, University College London, London, UK
2 Institute of Health Informatics, University College London, London, UK
3 Health Data Research UK London, University College London, London, UK
4 University College London British Heart Foundation Research Accelerator, London, UK
5 Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD), Medical Faculty & Faculty of Mathematics and Natural
Sciences, University of Cologne, Cologne, Germany
6 Institute of Cardiovascular Science, University College London, UK
7 Centre for Molecular Medicine, University of Cologne, Cologne, Germany
8 Max Planck Institute for Biology of Ageing, Cologne, Germany
Correspondence
Andreas Beyer, Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases (CECAD), Medical Faculty & Faculty of Mathematics and Natural Sciences, University of Cologne, Cologne, Germany.
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Linda Partridge, Institute of Healthy Ageing, Department of Genetics, Evolution and Environment, University College London, London, UK.
Email: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
Funding information
Bundesministerium für Bildung und Forschung, Grant/Award Number: HiGHmed 01ZZ1802U; UK Medical Research Council, Grant/Award Number: MR/N013867/1; Dunhill Medical Trust, Grant/Award Number: RPGF1806/67; BenevolentAI; Max- Planck-Gesellschaft; Wellcome Trust, Grant/Award Number: WT 110284/Z/15/Z; Deutsche Forschungsgemeinschaft, Grant/Award Number: CRC1310 and 325931972; British Heart Foundation, Grant/Award Number: AA/18/6/34223; European Research Council (ERC)
Abbreviations: AH, Aging hallmark; ARD, Age-related disease; EBI, European Bioinformatics Institute; ERK, Extracellular signal regulated kinase; GO, Gene Ontology; GSEA, Gene set
enrichment analysis; GWA, Genome-wide association; IFNg, Interferon gamma; MeSH, Medical Subject Headings; NCBI, National Centre for Biotechnology Information; NHGRI, National Human Genome Research Institute; PMID, PubMed unique Identifier; SNP, Single-nucleotide Polymorphism.
This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
© 2022 The Authors. Aging Cell published by Anatomical Society and John Wiley & Sons Ltd.
Abstract
Genetic, environmental, and pharmacological interventions into the aging process can confer resistance to multiple age-related diseases in laboratory animals, including rhesus monkeys. These findings imply that individual mechanisms of aging might contribute to the co-occurrence of age-related diseases in humans and could be targeted to prevent these conditions simultaneously. To address this question, we text mined 917,645 literature abstracts followed by manual curation and found strong, nonrandom associations between age-related diseases and aging mechanisms in humans, confirmed by gene set enrichment analysis of GWAS data. Integration of these associations with clinical data from 3.01 million patients showed that age-related diseases associated with each of five aging mechanisms were more likely than chance to be present together in patients. Genetic evidence revealed that innate and adaptive immunity, the intrinsic apoptotic signaling pathway and activity of the ERK1/2 pathway were associated with multiple aging mechanisms and diverse age-related diseases. Mechanisms of aging hence contribute both together and individually to age-related disease co-occurrence in humans and could potentially be targeted accordingly to prevent multimorbidity.
KEYWORDS
age-related disease, aging, aging hallmarks, genetics, multimorbidity
- 星期二, 03 9月 2024
The Hallmarks of Aging
Aging is characterized by a progressive loss of physiological integrity, leading to impaired function and increased vulnerability to death. This deterioration is the primary risk factor for major human pathologies, including cancer, diabetes, cardiovascular disorders, and neurodegenerative diseases. Aging research has experienced an unprecedented advance over recent years, particularly with the discovery that the rate of aging is controlled, at least to some extent, by genetic pathways and biochemical processes conserved in evolution. This Review enumerates nine tentative hallmarks that represent common denominators of aging in different organisms, with special emphasis on mammalian aging. These hallmarks are: genomic instability, telomere attrition, epigenetic alterations, loss of proteostasis, deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, and altered intercellular communication. A major challenge is to dissect the interconnectedness between the candidate hallmarks and their relative contributions to aging, with the final goal of identifying pharmaceutical targets to improve human health during aging, with minimal side effects.

- 星期一, 02 9月 2024
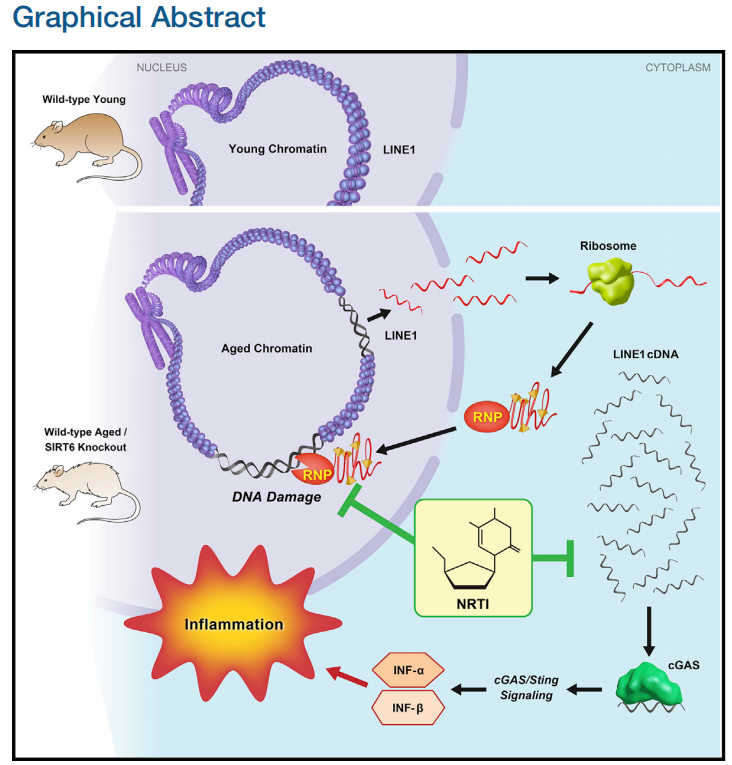
LINE1 Derepression in Aged Wild-Type and SIRT6- Deficient Mice Drives Inflammation
Authors
Matthew Simon, Michael Van Meter, Julia Ablaeva, ..., John M. Sedivy, Andrei Seluanov, Vera Gorbunova
Correspondence
该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (A.S.), 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (V.G.)
In Brief
Simon et al. show that LINE1 retrotransposon elements are derepressed in aged and progeroid mice. Cytoplasmic accumulation of LINE1 cDNA copies induced a type I interferon response, through the cGAS DNA sensing pathway, resulting in pathological inflammation. Inhibiting L1 replication significantly improved the health and lifespan of aged mice.
Highlights
● SIRT6 KO mice accumulate L1 cDNA, triggering interferon response via cGAS pathway
● Wild-type aged mice accumulate L1 cDNA and display type I interferon response
● Reverse-transcriptase inhibitors rescue type I interferon response and DNA damage
● Reverse-transcriptase inhibitors extend lifespan and improve health of SIRT6 KO mice
SUMMARY
Mice deficient for SIRT6 exhibit a severely shortened lifespan, growth retardation, and highly elevated LINE1 (L1) activity. Here we report that SIRT6-deficient cells and tissues accumulate abundant cytoplasmic L1 cDNA, which triggers strong type I interferon response via activation of cGAS. Remarkably, nucleoside reverse-transcriptase inhibitors (NRTIs), which inhibit L1 retrotransposition, significantly improved health and lifespan of SIRT6 knockout mice and completely rescued type I interferon response. In tissue culture, inhibition of L1 with siRNA or NRTIs abrogated type I interferon response, in addition to a significant reduction of DNA damage markers. These results indicate that L1 activation contributes to the pathologies of SIRT6 knockout mice. Similarly, L1 transcription, cytoplasmic cDNA copy number, and type I interferons were elevated in the wild-type aged mice. As sterile inflammation is a hallmark of aging, we propose that modulating L1 activity may be an important strategy for attenuating age-related pathologies.
Context and Significance
Mammalian aging is complex and likely reflects accumulated damage to our genes/DNA. Retrotransposons are a special class of parasitic genetic elements that can replicate their DNA within our genes, at times amounting to up to 20% of human DNA. Retrotransposons, such as the commonly occurring L1, have been associated with aging, neurodegeneration, and cancer. University of Rochester scientists uncovered L1 retrotransposons as the culprit in many aspects of accelerated aging in mice, a model for human aging. They also linked these special gene elements to inflammation. Experimentally blocking retrotransposon amplification improved the health and lifespan of mice. Although there is a long road ahead, inhibiting retrotransposon activity, and the related inflammation, could eventually be a therapy for age-related diseases.
- 星期五, 30 8月 2024
Cytoplasmic DNA: sources, sensing, and role in aging and disease
Karl N. Miller,1,6 Stella G. Victorelli,2,3,6 Hanna Salmonowicz,2,3,4,5 Nirmalya Dasgupta,1 Tianhui Liu,1 Joa˜o F. Passos,2,3,* and Peter D. Adams1,* 1Aging, Cancer and Immuno-oncology Program, Sanford Burnham Prebys Medical Discovery Institute, La Jolla, CA 92037, USA 2Department of Physiology and Biomedical Engineering, Mayo Clinic, Rochester, MN 55905, USA 3Robert and Arlene Kogod Center on Aging, Mayo Clinic, Rochester, MN 55905, USA 4Institute for Cell and Molecular Biosciences & Newcastle University Institute for Ageing, Newcastle upon Tyne NE4 5PL, UK 5International Institute of Molecular Mechanisms and Machines, Polish Academy of Sciences, 02-109 Warsaw, Poland 6These authors contributed equally
*Correspondence: 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (J.F.P.), 该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。 (P.D.A.)
https://doi.org/10.1016/j.cell.2021.09.034
SUMMARY
Endogenous cytoplasmic DNA (cytoDNA) species are emerging as key mediators of inflammation in diverse physiological and pathological contexts. Although the role of endogenous cytoDNA in innate immune activation is well established, the cytoDNA species themselves are often poorly characterized and difficult to distinguish, and their mechanisms of formation, scope of function and contribution to disease are incompletely understood. Here, we summarize current knowledge in this rapidly progressing field with emphases on similarities and differences between distinct cytoDNAs, their underlying molecular mechanisms of formation and function, interactions between cytoDNA pathways, and therapeutic opportunities in the treatment of age-associated diseases.
- 星期四, 29 8月 2024
In vivo partial cellular reprogramming enhances liver plasticity and regeneration
Graphical abstract
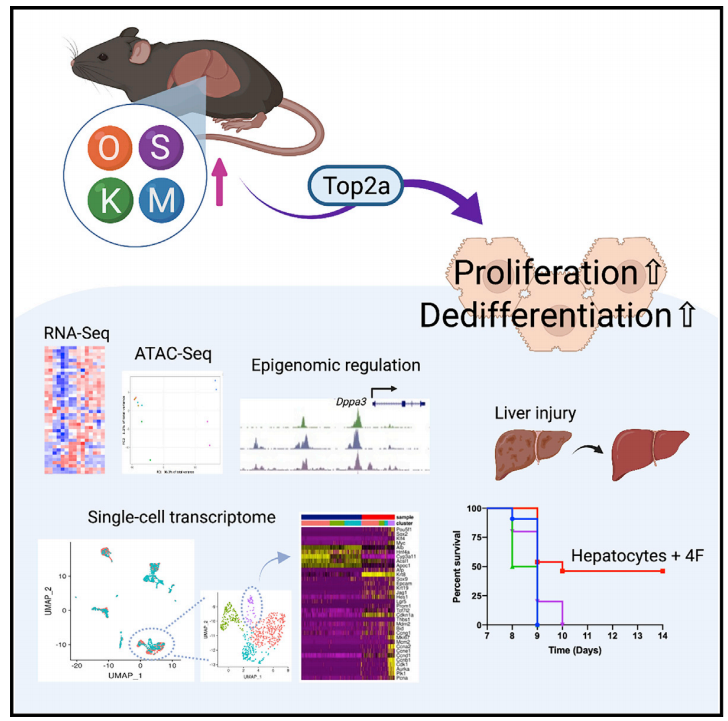
Highlights
Hepatocyte-specific 4F expression induces cell proliferation and dedifferentiation
Hepatocyte-specific 4F expression induces a global change in DNA accessibility
Top2a is required for cellular reprogramming in vitro and in vivo
In vivo reprogramming has beneficial effects on regenerative capacity
Authors
Tomoaki Hishida, Mako Yamamoto,
Yuriko Hishida-Nozaki, ...,
Pradeep Reddy, Guang-Hui Liu,
Juan Carlos Izpisua Belmonte
Correspondence
该Email地址已收到反垃圾邮件插件保护。要显示它您需要在浏览器中启用JavaScript。
In brief
In regenerating animals, such as fish and salamanders, dedifferentiation followed by proliferation contributes to tissue regeneration. Hishida et al. show that hepatocyte-specific cellular reprogramming induces cell proliferation and dedifferentiation in the liver and enhances liver regenerative capacity through topoisomerase2-mediated partial reprogramming.
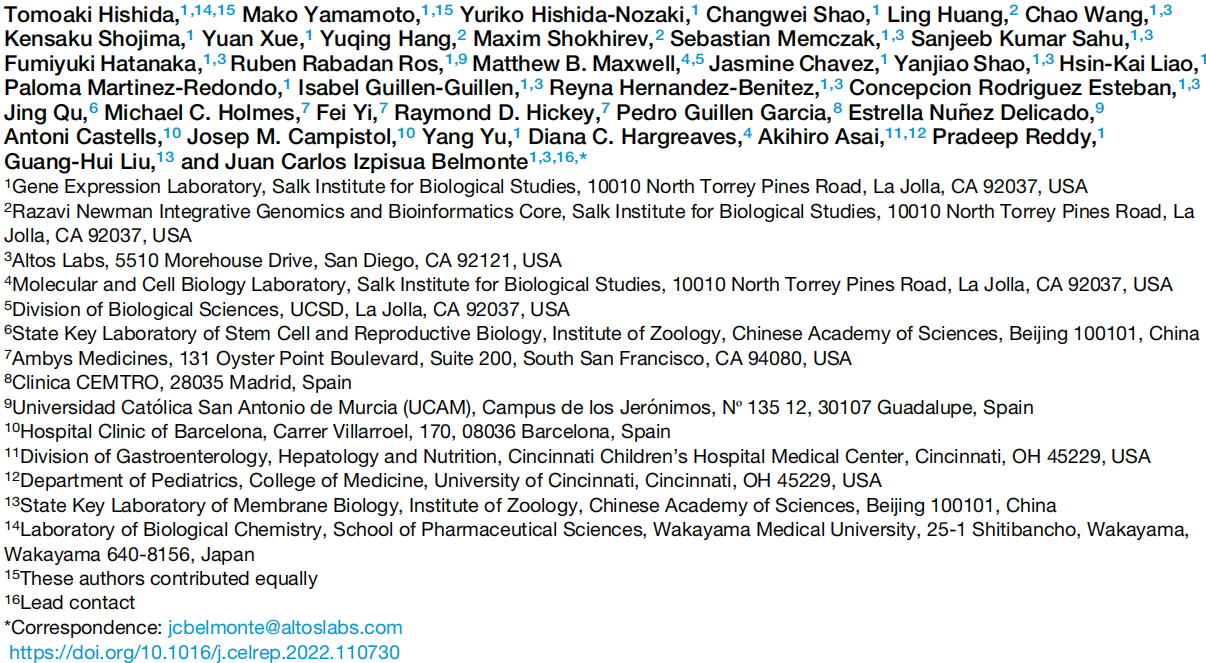
SUMMARY
Mammals have limited regenerative capacity, whereas some vertebrates, like fish and salamanders, are able to regenerate their organs efficiently. The regeneration in these species depends on cell dedifferentiation followed by proliferation. We generate a mouse model that enables the inducible expression of the four Yamanaka factors (Oct-3/4, Sox2, Klf4, and c-Myc, or 4F) specifically in hepatocytes. Transient in vivo 4F expression induces partial reprogramming of adult hepatocytes to a progenitor state and concomitantly increases cell proliferation. This is indicated by reduced expression of differentiated hepatic-lineage markers, an increase in markers of proliferation and chromatin modifiers, global changes in DNA accessibility, and an acquisition of liver stem and progenitor cell markers. Functionally, short-term expression of 4F enhances liver regenerative capacity through topoisomerase2-mediated partial reprogramming. Our results reveal that liver-specific 4F expression in vivo induces cellular plasticity and counteracts liver failure, suggesting that partial reprogramming may represent an avenue for enhancing tissue regeneration.
- 星期三, 28 8月 2024
The NADPARK study: A randomized phase I trial of nicotinamide riboside supplementation in Parkinson’s disease

SUMMARY
We conducted a double-blinded phase I clinical trial to establish whether nicotinamide adenine dinucleotide (NAD) replenishment therapy, via oral intake of nicotinamide riboside (NR), is safe, augments cerebral NAD levels, and impacts cerebral metabolism in Parkinson’s disease (PD). Thirty newly diagnosed, treatmentnaive patients received 1,000 mg NR or placebo for 30 days. NR treatment was well tolerated and led to a significant, but variable, increase in cerebral NAD levels—measured by 31phosphorous magnetic resonance spectroscopy—and related metabolites in the cerebrospinal fluid. NR recipients showing increased brain NAD levels exhibited altered cerebral metabolism, measured by 18fluoro-deoxyglucose positron emission to mography, and this was associated with mild clinical improvement. NR augmented the NAD metabolome and induced transcriptional upregulation of processes related to mitochondrial, lysosomal, and proteasomal function in blood cells and/or skeletal muscle. Furthermore, NR decreased the levels of inflammatory cytokines in serum and cerebrospinal fluid. Our findings nominate NR as a potential neuroprotective therapy for PD, warranting further investigation in larger trials.
