Implant related infection are the most common reason for implant failure accounting for about 2–5% of all orthopaedic surgeries (Shi et al, 2020). Implant related infection are caused by planktonic bacteria that adhere to the surface of the implant, where they proliferate and produce an extracellular polymeric substance (EPS), which encase the bacterial cluster increasing resistence to antibiotics (Arciola et al, 2014).
At the 2018, International Consensus Meeting (ICM) on Musculoskeletal infections states in orthopaedic trauma 1–30% cases may be infected. Open fractures are commonly associated with bacterial contamination rate up to 78.7% (Schwarz et al 2019; Seekamp et al, 2000).
Research focused on overcoming has implemented bycoating the surface of the implants with antibacterial materials that prevent biofilm formation (Campoccia et al, 2013). The most common substances used for coating an orthopaedic implant can be divided into anti-adhesive and bactericidal coatings. Anti-adhesive surfaces including polysaccharide coatings prevent biofilm formation. Antibiotics, chitosan (a natural polymer) and nanoparticles have also been used as a bactericidal coating (Junter et al, 2016). Prevention of bacterial adhesion and biofilm formation has reduced the implant related infection rates (Wang and Tang, 2019).
In recent years, Noble metal nanoparticles have been used as an alternative for the antibiotic coating. It is considered bioinert, anti-corrosive and biocompatible. Gold, silver, and palladium coatings give an osteointegrative and anti inflammatory effect. Antibiofilm coated implant (Orthosyn Intramedullary nail) are coated with these metals by covalently bonding them to the surface, providing stability and toxicological safety. These noble metals have different electro potentials, which gives a galvanic effect making it an antimicrobial coating.
Case 1
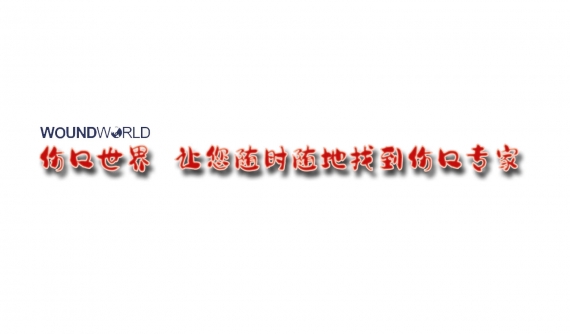
A 16-year-old girl with no known medical illness had an alleged Motor vehicle accident. She was unable to walk due to severe pain and deformity of the right thigh following the incident. She presented within three hours of the accident with a right open midshaft femur fracture (Figure 1). A lacerated puncture wound measuring 1x1 cm was seen over the proximal third of the right thigh. However, the neurovascular examination revealed normal findings.
As the patient presented within three hours, we proceeded with early definitive care, a definitive treatment for the long bones within 24 hours to 48 hours of initial trauma, to help the patient gain early mobility. After obtaining informed consent we went ahead with wound debridement and intramedullary nailing of the femur with an antibiofilm coated implant. The choice of the implant was to reduce the rate of infection postoperatively.
With the patient under general anesthesia, lying on a traction table, the lacerated wound was extended and debrided. The incision was given proximal to Greater Trochanter and dissected down to Greater Trochanter. A guidewire was inserted and positioned at the superior tip of the Greater Trochanter which was drilled under Image Intensifier (I/I) guidance. Proximal reaming of was femur done with size 13.5mm and a long guidewire inserted until the suprapatellar region. The size of the nail was measured after the reduction of the fracture. The femoral shaft was reamed in stages and the Intramedullary nail of the right femur, size 10 x 340mm was inserted. Proximal and distal screws were inserted using I/I guidance and wounds were washed and closed.
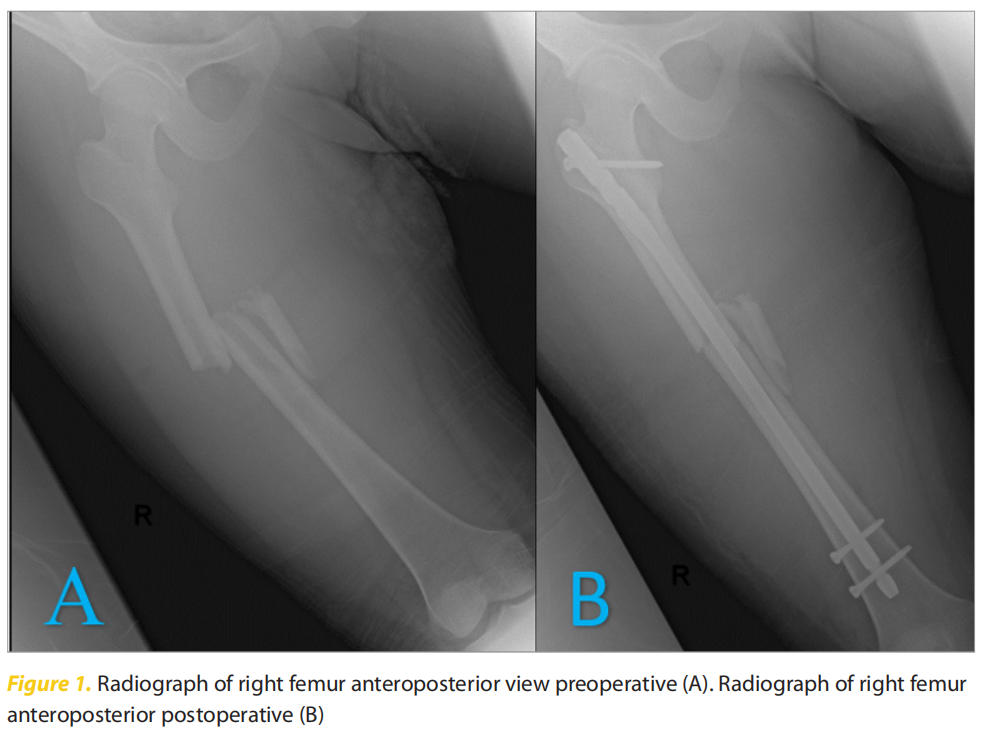
Postoperatively the patient was well with no signs of early infections at 6 months (Figure 2). The patient was able to walk without aid in 1-year follow-up with no signs of implant loosening or infection.
Case 2
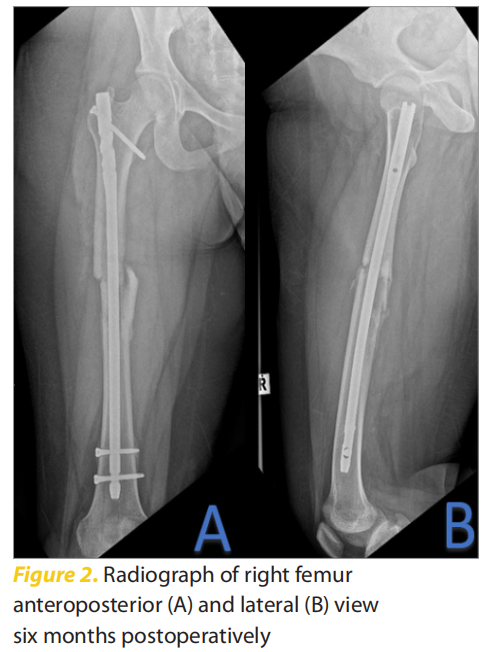
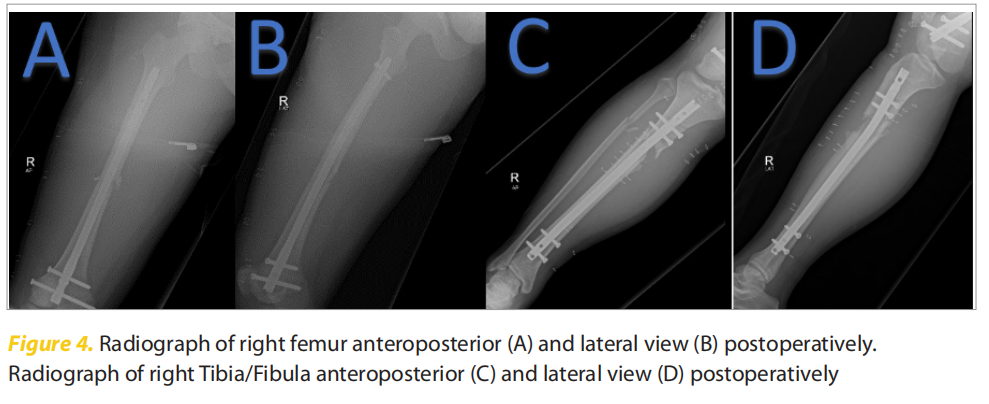
A 16-year-old male presented following an alleged motor vehicle accident with a closed displaced right midshaft femur fracture and closed right comminuted proximal third tibia fibula fracture (Figure 3). We proceeded with cross knee external fixation as the patient presented within 12 hours followed by retrograde interlocking femoral nail and antegrade interlocking nail tibia after seven days (Figure 4). This was complicated by surgical site infection (SSI), which was treated with culture-sensitive antibiotics after wound debridement. The patient was discharged 1-month postoperatively after the bacterial cultures were negative and the course of antibiotics was completed.

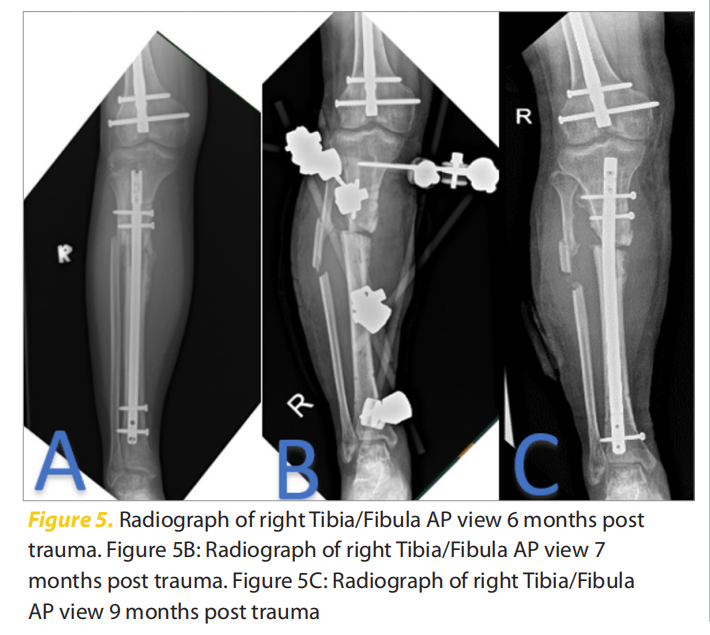
At two months he was allowed to partially bear weight. At six months postoperatively he presented with a septic nonunion with discharge from the surgical site. On the radiograph, there was the migration of the tibial Interlocking nail proximally with a delayed union (Figure 5). We proceeded with the removal of tibial implant and fibulectomy with acute docking delta external fixation of the leg (Figure 5B). Intraoperatively we noted a sinus communicating with the fracture, which is suggestive of osteomyelitis of the right tibia. The patient was given six weeks of antibiotics and discharged with a shoe raise of 4cm due to Limb Length discrepancy. At two months post-external fixation it was removed, and we put an antibiofilm coated implant (Orthosyn) (Figure 5C). Intraoperatively culture was Methicillin-resistant Staphylococcus aureus (MRSA), and he was started on a further six weeks of antibiotics.
After one year postoperatively he was able to fully bear weight with no complications with a range of motion of the knee 0 to 130 degrees (Figure 6). At two years follow up he was ambulating independently with no signs of infection.

Case 3
A 42-year obese gentleman with underlying Type II diabetes mellitus presented with a history of closed comminuted Subtrochanteric fracture of the left femur following a motor vehicle accident seven years ago. He was treated with interlocking nailing of left femur, subsequently after a one-year revision was done, because of the non-union with recon nail with cerclage wire of left femur with iliac bone graft. Dynamisation of the nail was done after five months because of nonunion of the left femur fracture. Given the fibrous nonunion of the fracture and hip pain post dynamization procedure, the implant was removed and a 9-hole proximal femur Locking plate with bone graft was inserted (Figure 7).

Following the surgery, he developed a surgical site infection in which the culture was MRSA positive. He was treated with antibiotics course of 21 days. The wound was closed with secondary suturing.
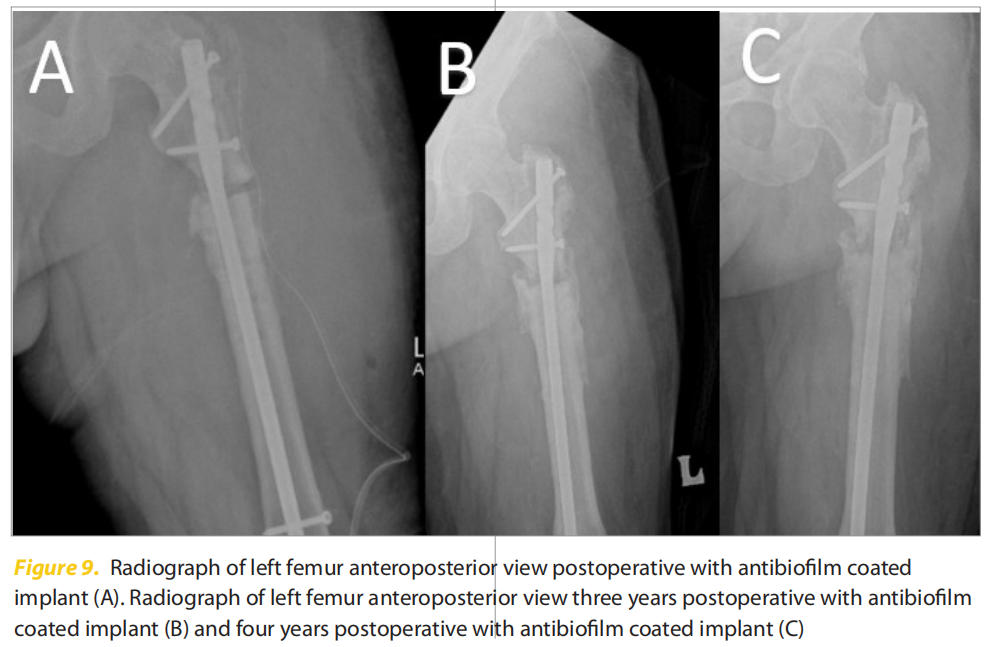
He sustained a trivial fall two years later and presented to our centre with pain and unable to bear weight. The radiograph shows a broken plate with loosening of all screws (Figure 8), which was removed, and subsequent cultures were sent followed by the insertion of an antibiofilm coated implant (Figure 9).
Postoperatively he had an apparent shortening of the left lower limb by 5cm with no pain. After four months postoperatively, he was able to walk with crutches with shoe raise. He had a delayed union of the left femur. He can ambulate with minimum support four years postoperatively with no signs of infection (Figure 9).

Discussion
In this case series, we have used antibiofilm coated implants in three different settings with good clinical outcomes. The first case for a Gustilo Anderson II was done within 12H post trauma with Bactiguard coated Interlocking nail with no signs of infection at a one-year period. The polytrauma case was complicated with SSIs post-treatment with a Bactiguard coated implant was able to ambulate with no signs of infection. Lastly, we presented an implant failure secondary to a delayed union. This was also treated with an antibiofilm-coated implant with a clinical union and a good clinical outcome four years after surgery.
Different types of coated implants have been used in orthopaedics, it’s a debatable concept as to which one is more superior over the other. A systemic review done by Savvidou et al (2020), on antimicrobial coated orthopaedic implants including 1307 patients concluded that antimicrobial coated implants significantly reduced the rate of implant-related infection postoperatively (Savvidou et al, 2020). ntimicrobial coated implants can be further elaborated to antibiotics, iodine coated, polymers, and noble metal nanoparticles coated implants.
Antibiotic coated, such as gentamicin-coated implants, have been used for their antibacterial effect. The risk of the development of antibiotic resistance has been a rising issue when using antibiotic coated implants (Wang and Tang, 2019). Gentamicin-coated implants are mainly used in complex and open fractures, severe soft tissue damage, and polytrauma patients with a good outcome, without gentamicin-related resistance or nephrotoxicity (Zagra et al, 2018).
Nanoparticles have been explored to see as an alternative to antibiotics for coating implants to kill bacteria and prevent biofilm formation (Webster and Taylor, 2011). Noble metal silver has been known for its antibacterial effect, but it has raised some health concerns regarding tissue toxicity from the silver coating (Shi et al, 2020). With the recent developments in implant manufacturing, silver is being more widely used by understandings its mechanism of action (Webster and Taylor, 2011). In which the silver nanoparticle coated implants have an antibiofilm action by changing the electroneutral charge of the surface, hence causing a galvanic effect (Mahamuni et al, 2019). Furthermore, Silver nanoparticles cause condensing of the bacterial DNA, and it loses the ability to replicate or through free radicle production generates a bactericidal effect (Webster and Taylor, 2011).
Palladium and gold nanoparticles are other noble metal that provides similar properties to silver in line with antibiofilm and anti bactericidal effect (Webster and Taylor, 2011). The strategy behind coating the implants is to change an inert surface to a biomaterial surface to prevent bacterial adhesion and biofilm formation, and coating with nanoparticles such as silver can encourage osteoblast function and osseointegration (Lamret et al, 2012). Noble metals are considered bioinert, corrosive resistant, and biocompatible. Gold and silver coating gives an osteointegration and antiinflammatory effect hence the mechanism of action is under discussion (Basova et al, 2021).
A combination of silver, gold, and platinum group metals has a synergistic effect and hence can be used as a biocompatible matrix. The two metals form a galvanic effect which oxidizes the more active component, which in turn controls silver ion release hence improving the biocidal effect (Basova et al, 2021; Vikulova et al, 2021).
In this case series, we used a Titanium implant coated with silver, gold, and palladium covalently bonded to the surface giving a galvanic effect. It was used on an open fracture as part of early total care, recurrent infection case, and a delayed union with good clinical and patient satisfaction.
Conclusion
Antibiofilm coated implants are a good option with good clinical outcome in treating orthopaedic implant related infections and delayed union.
References
1. Arciola C, Campoccia D, Ehrlich G, Montanaro L (2014) Biofilm-based implant infections in orthopaedics. Adv Exp Med Biol 830:29–46. https://doi.org/10.1007/978- 3-319-11038-7_2
2. Basova T, Vikulova E, Dorovskikh S et al (2021) The use of noble metal coatings and nanoparticles for the modification of medical implant materials. Materials & Design 204:109672. https://doi.org/10.1016/j. matdes.2021.109672
3. Campoccia D, Montanaro L, Arciola C (2013) A review of the biomaterials technologies for infection-resistant surfaces. Biomaterials 34(34):8533–54. 10.1016/j. biomaterials.2013.07.089
4. Junter G, Thébault P, Lebrun L (2016) Polysaccharide based antibiofilm surfaces. Acta Biomaterialia 30:13– 25. https://doi.org/10.1016/j.actbio.2015.11.010
5. Lamret F, Colin M, Mongaret C et al (2020) Antibiotic tolerance of Staphylococcus aureus biofilm in periprosthetic joint infections and antibiofilm Strategies. Antibiotics (Basel) 9(9):547. https://doi. org/10.3390/antibiotics9090547
6. Mahamuni P, Patil P, Dhanavade M et al (2019) Synthesis and characterization of zinc oxide nanoparticles by using polyol chemistry for their antimicrobial and antibiofilm activity. Biochemistry and Biophysics Reports 17:71-80. https://doi.org/10.1016/j. bbrep.2018.11.007
7. Savvidou O, Kaspiris A, Trikoupis I et al (2020) Efficacy of antimicrobial coated orthopaedic implants on the prevention of periprosthetic infections: a systematic review and meta-analysis. J Bone Jt Infect 5(4):212–22. https://doi.org/10.7150%2Fjbji.44839
8. Schwarz E, Parvizi J, Gehrke T et al (2019) 2018 International Consensus Meeting on musculoskeletal infection: research priorities from the general assembly questions. J Orthop Res 37(5):997–1006.w
9. Seekamp A, Köntopp H, Schandelmaier P et al (2000) Bacterial cultures and bacterial infection in open fractures. European Journal of Trauma 26(3):131–8
10. Shi R, Zhang J, Tian J et al (2020) An effective self powered strategy to endow titanium implant surface with associated activity of anti-biofilm and osteogenesis. Nano Energy 77:105201. https://doi. org/10.1016/j.nanoen.2020.105201
11. Wang M, Tang T (2019) Surface treatment strategies to combat implant-related infection from the beginning. J Orthop Translat 17:42–54. https://doi. org/10.1016/j.jot.2018.09.001
12. Vikulova E, Karakovskaya K, Koretskaya T et al (2021). MOCVD of noble metal film materials for medical implants: microstructure and biocompatibility of Ir and Au/Ir Coatings on TiNi. Coatings 11(6):638. https://doi.org/10.3390/coatings11060638
13. Webster T, Taylor (2011) Reducing infections through nanotechnology and nanoparticles. Int J Nanomedicine 6:1463–73. https://doi.org/10.2147/ ijn.s22021
14. Zagra L, Gallazzi E, Romanò D et al (2018) Two-stage cementless hip revision for peri-prosthetic infection with an antibacterial hydrogel coating: results of a comparative series. Int Orthop 43(1):111–5. https:// doi.org/10.1007/s00264-018-4206-2
This article is excerpted from the Wounds Asia 2022 | Vol 5 Issue 1 by Wound World.