文献精选
摘自:中华普通外科杂志 2017 年 9 月第 32 卷第 9 期
作者:中华医学会外科学分会血管外科学组
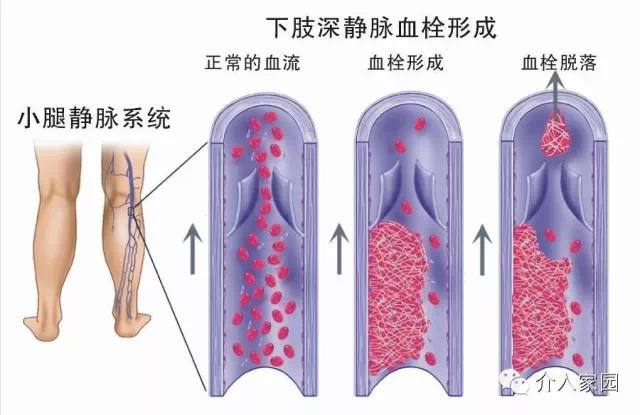
深静脉血检形成(DVT)是血液在深静脉内不正常凝结引起的静脉回流障碍性疾病,常发生于下肢。血栓脱落可引起肺动脉栓塞(PE),DVT与PE统称为静脉血栓栓塞症(VTE),是同种疾病在不同阶段的表现形式。DVT的主要不良后果是PE和血栓后综合征(PTS),它可以显著影响患者的生活质量,甚至导致死亡。因此,为了提高我国DVT的诊治水平,指导和规范各级医院对DVT的诊治工作,特制订本指南。
55岁的李先生近来老感觉腿痒,就自己到药店买了些药膏每天涂抹,可一个月过去了,情况非但没有好转,反而严重了。家人带她去医院皮肤科做了检查,医生详细问诊后建议她去血管外科就诊,经血管外科会诊确诊为静脉曲张。
[摘要] 目的:分析造口底盘在造口旁切口治疗中的应用效果。 方法:纳入 2018 年 11 月至 2019 年 11 月我院外 科造口门诊 60 例造口与切口距离<底盘覆盖范围(10 cm×10 cm)的病人,随机分为研究组和对照组各 30 例。 研究组 使用造口底盘,对照组采用片状水胶体敷料治疗保护。 评价两组病人治疗效果、舒适度、换药时间和成本效益的差 异。 结果:研究组和对照组回肠造口分别为 23 例、21 例,结肠造口分别为 7 例、9 例。 研究组和对照组造口周围皮肤 变色、侵蚀和组织增生的评分分别为(5.67±1.21)和(5.80±1.24),切口面积分别为(18.76±16.14) cm2 和(20.91±15.39) cm2 。 两组病人 7 d 后治疗效果和舒适度比较,差异无统计学意义。 但研究组的治疗成本低于对照组[(244.67±58.47)元比 (341.43±106.13)元,P<0.001],换药时间亦少于对照组[(10.90±1.58) min 比(14.77±3.42) min,P<0.001),差 异 均 有 显著统计学意义。 结论:造口底盘可替代水胶体对造口旁切口进行治疗和保护,为造口旁切口治疗的方法之一。
关键词:造口底盘; 切口愈合; 应用效果




