文献精选




This article is excerpted from the 《Frontiers in Physiology》 by Wound World



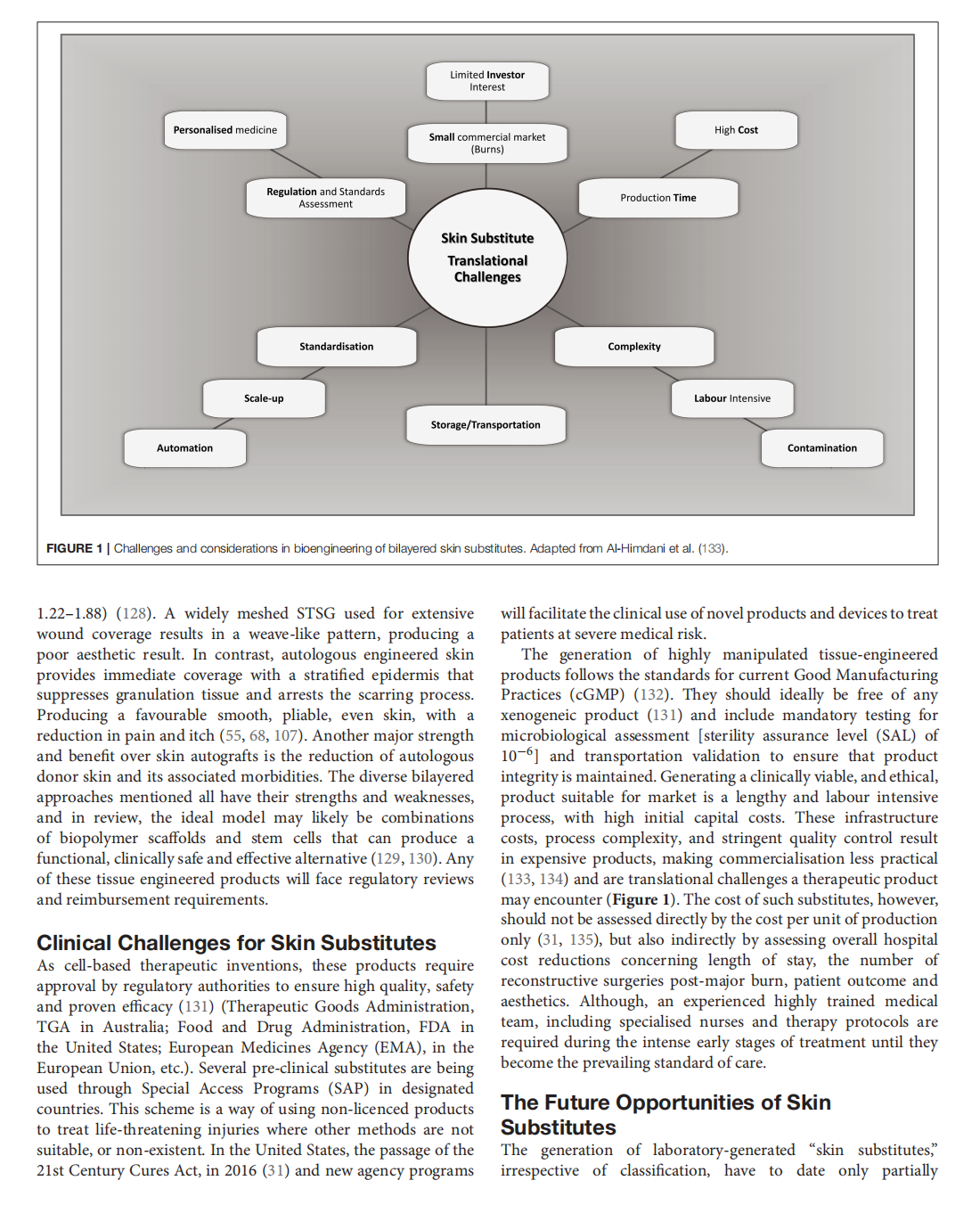



This article is excerpted from the《Frontiers in Surgery》by Wound World

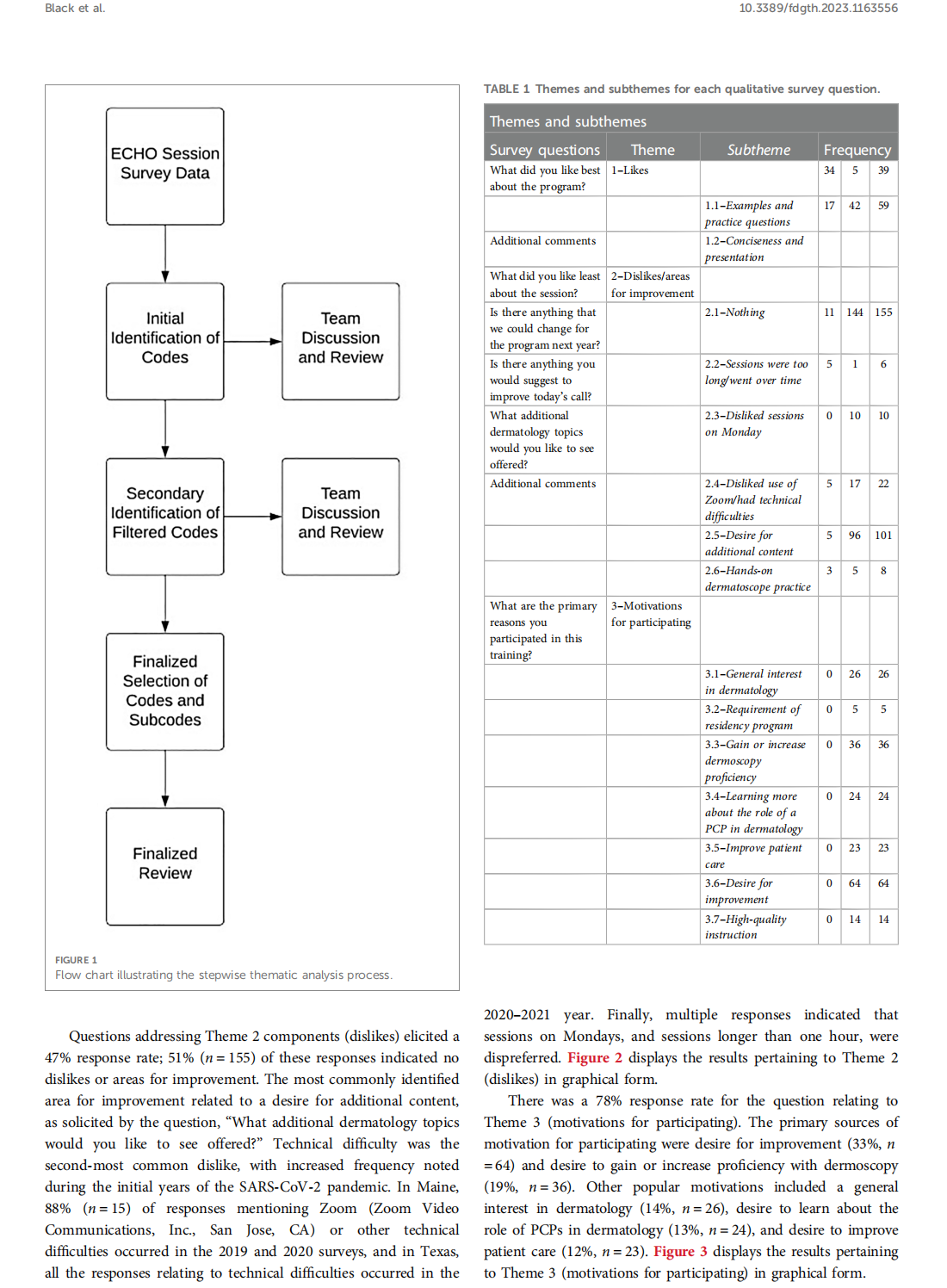
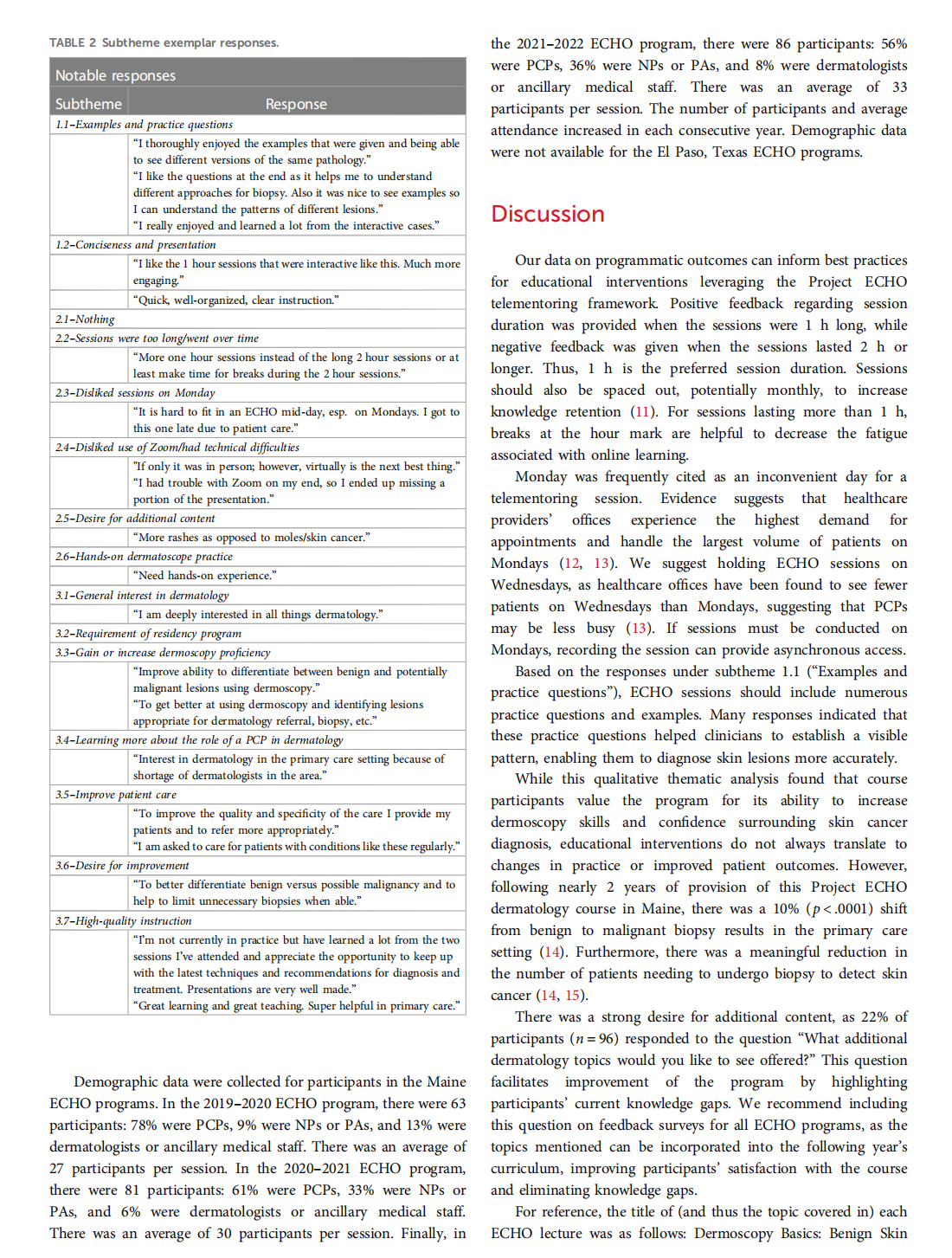

This article is excerpted from the 《Frontiers in Digital Health》 by Wound World
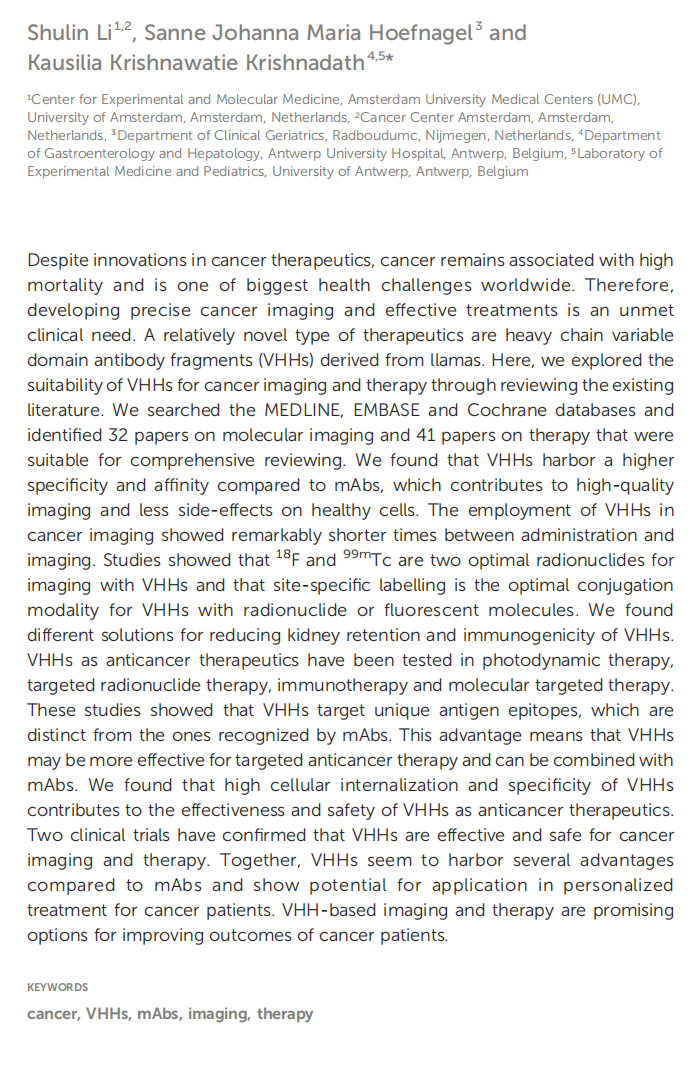










This article is excerpted from the 《Frontiers in Oncology》 by Wound World